Current Biotechnology ›› 2024, Vol. 14 ›› Issue (5): 793-804.DOI: 10.19586/j.2095-2341.2024.0078
• Reviews • Previous Articles Next Articles
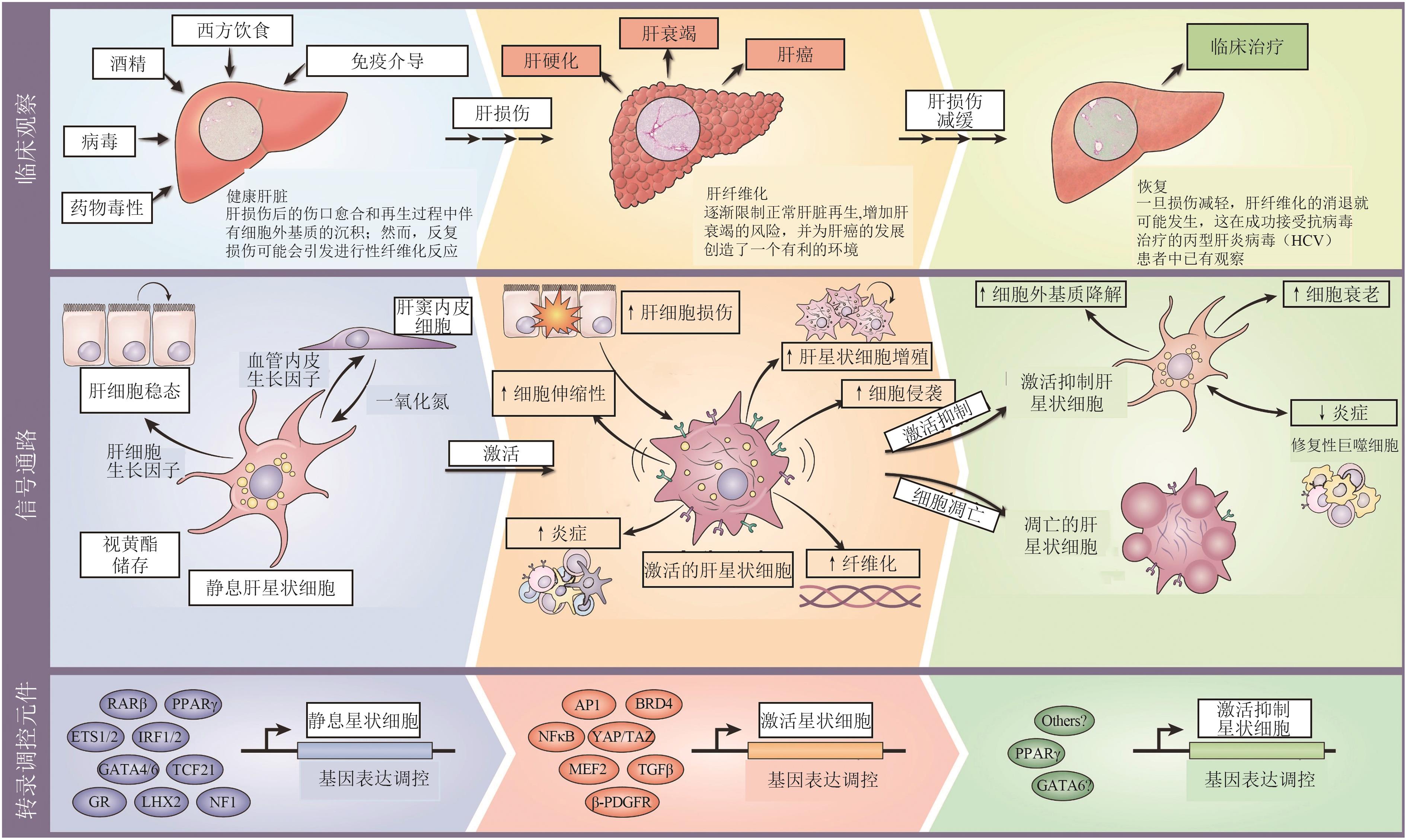
Research Progress of Single-cell Transcriptome Sequencing Technology in Liver Fibrosis
Lingfei WAN( ), Wenting PAN, Yuting YONG, Yuanshuai LI, Yue ZHAO, Xinlong YAN(
), Wenting PAN, Yuting YONG, Yuanshuai LI, Yue ZHAO, Xinlong YAN( )
)
- College of Chemistry and Life Science,Beijing University of Technology,Beijing 100124,China
-
Received:2024-04-11Accepted:2024-07-02Online:2024-09-25Published:2024-10-22 -
Contact:Xinlong YAN
单细胞转录组测序技术在肝纤维化中的研究进展
万令飞( ), 潘文婷, 雍雨婷, 李元帅, 赵悦, 阎新龙(
), 潘文婷, 雍雨婷, 李元帅, 赵悦, 阎新龙( )
)
- 北京工业大学化学与生命科学学院,北京 100124
-
通讯作者:阎新龙 -
作者简介:万令飞 E-mail: wan-lingfei@outlook.com; -
基金资助:北京市自然科学基金和市教委基金联合基金重点项目(KZ202210005010);中国博士后科学基金(2023M740168);北京市博士后科研活动基金(2023-22-23)
CLC Number:
Cite this article
Lingfei WAN, Wenting PAN, Yuting YONG, Yuanshuai LI, Yue ZHAO, Xinlong YAN. Research Progress of Single-cell Transcriptome Sequencing Technology in Liver Fibrosis[J]. Current Biotechnology, 2024, 14(5): 793-804.
万令飞, 潘文婷, 雍雨婷, 李元帅, 赵悦, 阎新龙. 单细胞转录组测序技术在肝纤维化中的研究进展[J]. 生物技术进展, 2024, 14(5): 793-804.
share this article
| 1 | HAMMEL P, COUVELARD A, O'TOOLE D, et al.. Regression of liver fibrosis after biliary drainage in patients with chronic pancreatitis and stenosis of the common bile duct[J]. N. Engl. J. Med., 2001, 344(6): 418-423. |
| 2 | KWEON Y O, GOODMAN Z D, DIENSTAG J L, et al.. Decreasing fibrogenesis: an immunohistochemical study of paired liver biopsies following lamivudine therapy for chronic hepatitis B[J]. J. Hepatol., 2001, 35(6): 749-755. |
| 3 | ARTHUR M J P. Reversibility of liver fibrosis and cirrhosis following treatment for hepatitis C[J]. Gastroenterology, 2002, 122(5): 1525-1528. |
| 4 | CZAJA A J, CARPENTER H A. Decreased fibrosis during corticosteroid therapy of autoimmune hepatitis[J]. J. Hepatol., 2004, 40(4): 646-652. |
| 5 | DIXON J B, BHATHAL P S, HUGHES N R, et al.. Nonalcoholic fatty liver disease: improvement in liver histological analysis with weight loss[J]. Hepatology, 2004, 39(6): 1647-1654. |
| 6 | BURT A D. Liver fibrosis[J]. Br. Med. J., 1992, 305(6853):537-538. |
| 7 | HERNANDEZ-GEA V, FRIEDMAN S L. Pathogenesis of liver fibrosis[J]. Ann. Rev. Pathol. Mechan. Disease, 2011, 6(1):425-456. |
| 8 | ROCKEY D C, BELL P D, HILL J A. Fibrosis: a common pathway to organ injury and failure[J]. N. Engl. J. Med., 2015, 372(12): 1138-1149. |
| 9 | WANG S, FRIEDMAN S L. Hepatic fibrosis: a convergent response to liver injury that is reversible[J]. J. Hepatol., 2020, 73(1): 210-211. |
| 10 | DREW L. Tipping the balance[J/OL]. Nature, 2018, 564(7736): S74-S75[2024-05-13]. . |
| 11 | 杨瑞华,李芹,陈玮.扶正化瘀胶囊治疗慢性乙型肝炎肝纤维化疗效的Meta分析[J].中华肝脏病杂志,2015,23(4):295-296. |
| YANG R H, LI Q, CHEN W. Efficacy and safety of Fuzhenghuayu capsule for treating liver fibrosis in patients with chronic hepatitis B: a meta-analysis[J]. Chin. J. Hepatol., 2015, 23(4): 295-296. | |
| 12 | 苗亮,杨婉娜,董晓琴,等.安络化纤丸联合恩替卡韦治疗可显著提高慢性乙型肝炎病毒感染者肝纤维化的改善率[J].中华肝脏病杂志,2019,27(7):521-526. |
| MIAO L, YANG W N, DONG X Q, et al.. Combined anluohuaxianwan and entecavir treatment significantly improve the improvement rate of liver fibrosis in patients with chronic hepatitis B virus infection[J]. Chin. J. Hepatol., 2019, 27(7): 521-526. | |
| 13 | JI D, CHEN Y, BI J, et al.. Entecavir plus Biejia-Ruangan compound reduces the risk of hepatocellular carcinoma in Chinese patients with chronic hepatitis B[J]. J. Hepatol., 2022, 77(6): 1515-1524. |
| 14 | LIU Y Q, ZHANG C, LI J W, et al.. An-Luo-Hua-Xian pill improves the regression of liver fibrosis in chronic hepatitis B patients treated with entecavir[J]. J. Clin. Transl. Hepatol., 2023, 11(2): 304-313. |
| 15 | NEUSCHWANDER-TETRI B A. Targeting the FXR nuclear receptor to treat liver disease[J]. Gastroenterology, 2015, 148(4): 704-706. |
| 16 | HARRISON S A, RINELLA M E, ABDELMALEK M F, et al.. NGM282 for treatment of non-alcoholic steatohepatitis: a multicentre, randomised, double-blind, placebo-controlled, phase 2 trial[J]. Lancet, 2018, 391(10126): 1174-1185. |
| 17 | QIAN T, FUJIWARA N, KONERU B, et al.. Molecular signature predictive of long-term liver fibrosis progression to inform antifibrotic drug development[J]. Gastroenterology, 2022, 162(4): 1210-1225. |
| 18 | TANG F, BARBACIORU C, WANG Y, et al.. mRNA-Seq whole-transcriptome analysis of a single cell[J]. Nat. Methods, 2009, 6(5): 377-382. |
| 19 | GAWAD C, KOH W, QUAKE S R. Single-cell genome sequencing: current state of the science[J]. Nat. Rev. Genet., 2016, 17(3): 175-188. |
| 20 | TANAY A, REGEV A. Scaling single-cell genomics from phenomenology to mechanism[J]. Nature, 2017, 541(7637): 331-338. |
| 21 | BASLAN T, HICKS J. Unravelling biology and shifting paradigms in cancer with single-cell sequencing[J]. Nat. Rev. Cancer, 2017, 17(9): 557-569. |
| 22 | VAN DE SANDE B, LEE J S, MUTASA-GOTTGENS E, et al.. Applications of single-cell RNA sequencing in drug discovery and development[J]. Nat. Rev. Drug Discov., 2023, 22(6): 496-520. |
| 23 | QUAIL M A, KOZAREWA I, SMITH F, et al.. A large genome center's improvements to the Illumina sequencing system[J]. Nat. Methods, 2008, 5(12): 1005-1010. |
| 24 | HAO Y, STUART T, KOWALSKI M H, et al.. Dictionary learning for integrative, multimodal and scalable single-cell analysis[J]. Nat. Biotechnol., 2024, 42(2): 293-304. |
| 25 | WOLF F A, ANGERER P, THEIS F J. SCANPY large-scale single-cell gene expression data analysis[J/OL]. Genome Biol., 2018, 19(1): 15[2024-05-13]. . |
| 26 | ZHENG G X, TERRY J M, BELGRADER P, et al.. Massively parallel digital transcriptional profiling of single cells[J/OL]. Nat. Commun., 2017, 8: 14049[2024-05-13]. . |
| 27 | TRAPNELL C, CACCHIARELLI D, GRIMSBY J, et al.. The dynamics and regulators of cell fate decisions are revealed by pseudotemporal ordering of single cells[J]. Nat. Biotechnol., 2014, 32(4): 381-386. |
| 28 | FRIEDMAN S L. Hepatic stellate cells: protean, multifunctional, and enigmatic cells of the liver[J]. Physiol. Rev., 2008, 88(1): 125-172. |
| 29 | SHERMAN M H. Stellate cells in tissue repair, inflammation, and cancer[J]. Annu. Rev. Cell Dev. Biol., 2018, 34: 333-355. |
| 30 | TSUCHIDA T, FRIEDMAN S L. Mechanisms of hepatic stellate cell activation[J]. Nat. Rev. Gastroenterol. Hepatol., 2017, 14(7): 397-411. |
| 31 | BAGHAEI K, MAZHARI S, TOKHANBIGLI S, et al.. Therapeutic potential of targeting regulatory mechanisms of hepatic stellate cell activation in liver fibrosis[J]. Drug Discov. Today, 2022, 27(4): 1044-1061. |
| 32 | WANG S S, TANG X T, LIN M, et al.. Perivenous stellate cells are the main source of myofibroblasts and cancer-associated fibroblasts formed after chronic liver injuries[J]. Hepatology, 2021, 74(3): 1578-1594. |
| 33 | KRENKEL O, HUNDERTMARK J, RITZ T P, et al.. Single cell RNA sequencing identifies subsets of hepatic stellate cells and myofibroblasts in liver fibrosis[J/OL]. Cells, 2019, 8(5): 503[2024-05-13]. . |
| 34 | TSUCHIYA Y, SEKI T, KOBAYASHI K, et al.. Fibroblast growth factor 18 stimulates the proliferation of hepatic stellate cells, thereby inducing liver fibrosis[J/OL]. Nat. Commun., 2023, 14(1): 6304[2024-05-13]. . |
| 35 | ROSENTHAL S B, LIU X, GANGULY S, et al.. Heterogeneity of HSCs in a mouse model of NASH[J]. Hepatology, 2021, 74(2): 667-685. |
| 36 | LEI L, BRUNEAU A, MOURABIT H E L, et al.. Portal fibroblasts with mesenchymal stem cell features form a reservoir of proliferative myofibroblasts in liver fibrosis[J]. Hepatology, 2022, 76(5): 1360-1375. |
| 37 | IWANO M, PLIETH D, DANOFF T M, et al.. Evidence that fibroblasts derive from epithelium during tissue fibrosis[J]. J. Clin. Invest., 2002, 110(3): 341-350. |
| 38 | OMENETTI A, PORRELLO A, JUNG Y, et al.. Hedgehog signaling regulates epithelial-mesenchymal transition during biliary fibrosis in rodents and humans[J]. J. Clin. Invest., 2008, 118(10): 3331-3342. |
| 39 | TAURA K, MIURA K, IWAISAKO K, et al.. Hepatocytes do not undergo epithelial-mesenchymal transition in liver fibrosis in mice[J]. Hepatology, 2010, 51(3): 1027-1036. |
| 40 | CHU A S, DIAZ R, HUI J J, et al.. Lineage tracing demonstrates no evidence of cholangiocyte epithelial-to-mesenchymal transition in murine models of hepatic fibrosis[J]. Hepatology, 2011, 53(5): 1685-1695. |
| 41 | ZHU C, KIM K, WANG X, et al.. Hepatocyte Notch activation induces liver fibrosis in nonalcoholic steatohepatitis[J/OL]. Sci. Transl. Med., 2018, 10(468): eaat0344[2024-05-13]. . |
| 42 | WANG G, DUAN J, PU G, et al.. The Annexin A2-Notch regulatory loop in hepatocytes promotes liver fibrosis in NAFLD by increasing osteopontin expression[J/OL]. Biochim. Biophys. Acta Mol. Basis Dis., 2022, 1868(8): 166413[2024-05-13]. . |
| 43 | SCHULIEN I, HOCKENJOS B, SCHMITT-GRAEFF A, et al.. The transcription factor c-Jun/AP-1 promotes liver fibrosis during non-alcoholic steatohepatitis by regulating Osteopontin expression[J]. Cell Death Differ., 2019, 26(9): 1688-1699. |
| 44 | RAMACHANDRAN P, DOBIE R, WILSON-KANAMORI J R, et al.. Resolving the fibrotic niche of human liver cirrhosis at single-cell level[J]. Nature, 2019, 575(7783): 512-518. |
| 45 | ZHANG S, WAN D, ZHU M, et al.. CD11b+CD43hi Ly6Clo splenocyte-derived macrophages exacerbate liver fibrosis via spleen-liver axis[J]. Hepatology, 2023, 77(5): 1612-1629. |
| 46 | MENG X M, WANG S, HUANG X R, et al.. Inflammatory macrophages can transdifferentiate into myofibroblasts during renal fibrosis[J/OL]. Cell Death Dis., 2016, 7(12): e2495[2024-05-12]. . |
| 47 | WANG Y Y, JIANG H, PAN J, et al.. Macrophage-to-myofibroblast transition contributes to interstitial fibrosis in chronic renal allograft injury[J]. J. Am. Soc. Nephrol., 2017, 28(7): 2053-2067. |
| 48 | LITTLE K, LLORIÁN-SALVADOR M, TANG M, et al.. Macrophage to myofibroblast transition contributes to subretinal fibrosis secondary to neovascular age-related macular degeneration[J/OL]. J. Neuroinflam., 2020, 17(1): 355[2024-05-13]. . |
| 49 | ZHAO J, ZHANG S, LIU Y, et al.. Single-cell RNA sequencing reveals the heterogeneity of liver-resident immune cells in human[J/OL]. Cell Discov., 2020, 6: 22[2024-05-13]. . |
| 50 | ZHANG Y, LI J, LI H, et al.. Single-cell RNA sequencing to dissect the immunological network of liver fibrosis in Schistosoma japonicum-infected mice[J/OL]. Front. Immunol., 2022, 13: 980872[2024-05-13]. . |
| 51 | SCHLEDZEWSKI K, GÉRAUD C, ARNOLD B, et al.. Deficiency of liver sinusoidal scavenger receptors stabilin-1 and-2 in mice causes glomerulofibrotic nephropathy via impaired hepatic clearance of noxious blood factors[J]. J. Clin. Invest., 2011, 121(2): 703-714. |
| 52 | POISSON J, LEMOINNE S, BOULANGER C, et al.. Liver sinusoidal endothelial cells: physiology and role in liver diseases[J]. J. Hepatol., 2017, 66(1): 212-227. |
| 53 | SHETTY S, LALOR P F, ADAMS D H. Liver sinusoidal endothelial cells-gatekeepers of hepatic immunity[J]. Nat. Rev. Gastroenterol. Hepatol., 2018, 15(9): 555-567. |
| 54 | MARRONE G, SHAH V H, GRACIA-SANCHO J. Sinusoidal communication in liver fibrosis and regeneration[J]. J. Hepatol., 2016, 65(3): 608-617. |
| 55 | MACPARLAND S A, LIU J C, MA X Z, et al.. Single cell RNA sequencing of human liver reveals distinct intrahepatic macrophage populations[J/OL]. Nat. Commun., 2018, 9(1): 4383[2024-05-13]. . |
| 56 | HALPERN K B, SHENHAV R, MASSALHA H, et al.. Paired-cell sequencing enables spatial gene expression mapping of liver endothelial cells[J]. Nat. Biotechnol., 2018, 36(10): 962-970. |
| 57 | ZEISBERG E M, TARNAVSKI O, ZEISBERG M, et al.. Endothelial-to-mesenchymal transition contributes to cardiac fibrosis[J]. Nat. Med., 2007, 13(8): 952-961. |
| 58 | ZHANG Y, WU X, LI Y, et al.. Endothelial to mesenchymal transition contributes to arsenic-trioxide-induced cardiac fibrosis[J/OL]. Sci. Rep., 2016, 6: 33787[2024-05-13]. . |
| 59 | GONZALES J, HOLBERT K, CZYSZ K, et al.. Hemin-induced endothelial dysfunction and endothelial to mesenchymal transition in the pathogenesis of pulmonary hypertension due to chronic hemolysis[J/OL]. Int. J. Mol. Sci., 2022, 23(9): 4763[2024-05-13]. . |
| 60 | NIE X, WU Z, SHANG J, et al.. Curcumol suppresses endothelial-to-mesenchymal transition via inhibiting the AKT/GSK3β signaling pathway and alleviates pulmonary arterial hypertension in rats[J/OL]. Eur. J. Pharmacol., 2023, 943: 175546[2024-05-13]. . |
| 61 | SHI Z, ZHANG K, CHEN T, et al.. Transcriptional factor ATF3 promotes liver fibrosis via activating hepatic stellate cells[J/OL]. Cell Death Dis., 2020, 11(12): 1066[2024-05-13]. . |
| 62 | HALPERN K B, SHENHAV R, MATCOVITCH-NATAN O, et al.. Single-cell spatial reconstruction reveals global division of labour in the mammalian liver[J]. Nature, 2017, 542(7641): 352-356. |
| 63 | DOBIE R, WILSON-KANAMORI J R, HENDERSON B E P, et al.. Single-cell transcriptomics uncovers zonation of function in the mesenchyme during liver fibrosis[J]. Cell Rep., 2019, 29(7): 1832-1847.e8. |
| 64 | 王惠,赵鹏翔,张旭娟,等.间充质干细胞在疾病治疗中的应用潜力[J].生物技术进展,2021,11(6):688-693. |
| WANG H, ZHAO P X, ZHANG X J, et al.. The application potential of mesenchymal stem cells in the treatment of diseases[J]. Curr. Biotechnol., 2021, 11(6): 688-693. |
| [1] | Lingfei WAN, Wenting PAN, Yuting YONG, Yuanshuai LI, yue ZHAO, Xinlong YAN. Research Progress in Spatial Transcriptomics Technology for Liver Disease Research [J]. Current Biotechnology, 2025, 15(4): 645-654. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||